Laser Treatment for Nail Fungus Miami
At Luxe Foot Surgery in Miami, we provide excellent laser treatment for nail fungus. Our dermatology specialists will diagnose your condition and recommend the most suitable treatment. With modern and comfortable facilities, we prioritize your comfort during your visit. We believe in ethical, compassionate, and professional care from day one.
- Updated on: January 16, 2024
AVERAGE COST
$1,500
PROCEDURE TIME
20 – 40 Min
BACK TO WORK
1 week
FULL RECOVERY
2 weeks
Book Your Free Consultation

What is laser treatment for nail fungus?
Laser treatment for nail fungus is a non-invasive and highly effective procedure aimed at eliminating fungal infections in the nails. It utilizes laser technology to target and destroy the fungus without causing damage to the surrounding healthy tissue. During the treatment, the laser emits a focused beam of light that penetrates the nail, targeting the fungus and inhibiting its growth. The laser energy heats up and destroys the fungal cells, effectively eradicating the infection.
Laser treatment for nail fungus is known for its high success rate and minimal side effects. It is a safe and convenient option for individuals seeking a fast and efficient solution to their nail fungus problems.
What is onychomycosis or toenail fungus infection?
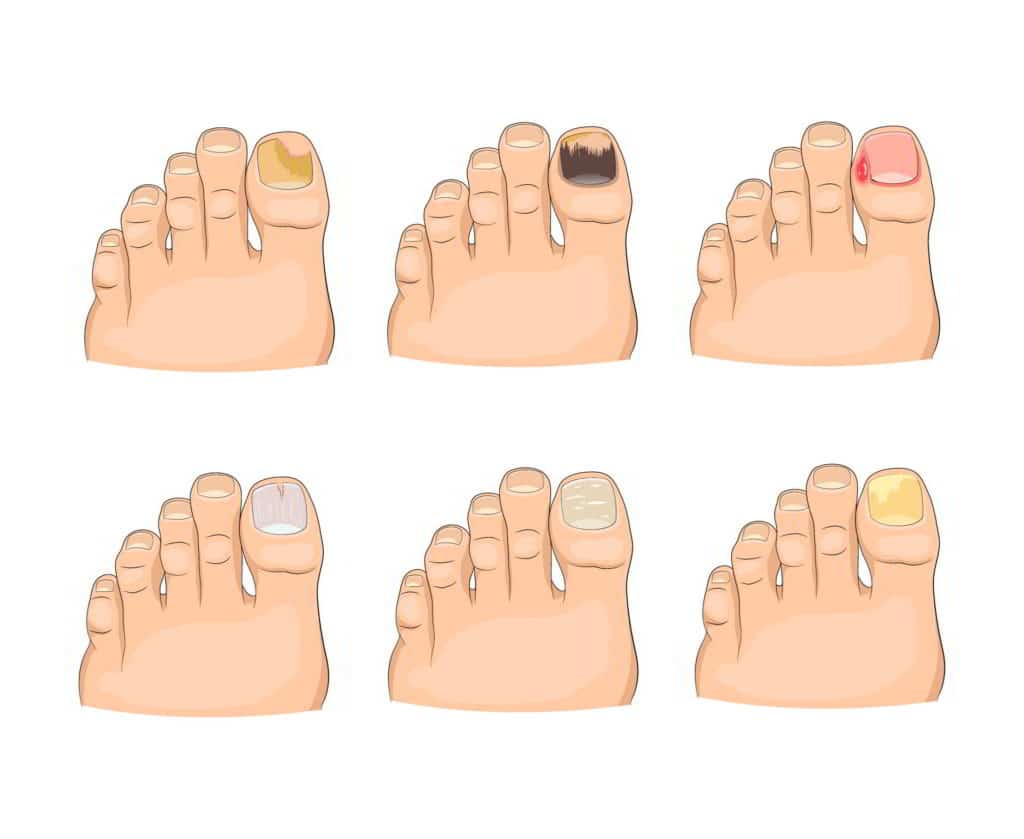
Onychomycosis, also known as toenail fungus infection, is a type of fungal infection that affects the nails. Normally, toenails have a pinkish, shiny, smooth, and uniform appearance. However, when nails are attacked by fungi, they can become discolored, turning yellowish, whitish, or brown. They may also become thick, brittle, and slightly painful or uncomfortable. While this type of infection is not considered serious, it can be challenging to eliminate. Onychomycosis is a common term used to describe fungal infection in the toenails.
Global prevalence of toenail fungus infection
Onychomycosis is a fairly common condition, accounting for 50% of all nail disorders worldwide. Despite improvements in quality of life and personal hygiene measures, toenail fungus infection is increasing globally. Statistics indicate that approximately 2% to 3% of the US population suffers from toenail fungus infection, although it is believed that these numbers underestimate the true prevalence. The incidence of this condition is higher in males than females, and it is more common in older adults, with 30% of affected individuals being over 60 years old. However, it can occur at any stage of life, even in children under 16 years old. It is estimated that between 0.2% and 2.6% of individuals with toenail fungus infection are children and adolescents.

Cost of Nail Fungus Treatment in Miami: Factors and Pricing Options
The cost of nail fungus treatment in Miami varies depending on the type of treatment administered to the patient. In recent years, laser treatment for nail fungus has shown to be one of the most effective options. The approximate price for this treatment depends on the number of sessions required and the number of affected toes. The more toes involved, the higher the fee, and the more complex the fungus, the more sessions the patient may need. The general cost, including the session and consultation with the doctor, would range from $500 to $1000 for 4 sessions and 5 toes.
Oral treatment for nail fungus can be more expensive than laser treatment. Patients may spend between $1000 and $1500 on this type of treatment. Topical ointments and nail polishes are usually the most economical options; however, they may be less effective, and the fungus may not completely disappear with these treatments.
Anatomy of the Nails
To understand how fungi attack and affect toenails, it is important to comprehend the anatomy of the nails. A nail is composed of three parts: the matrix, the nail plate, and the nail bed.
Matrix:
The matrix is the root of the nail and includes the lunula, which is the crescent-shaped, often differently colored part of the nail. It is located at the distal end of the matrix.
Nail Plate:
The nail plate is what we typically recognize as the visible nail. It consists of layers of keratinized cells. The outermost layer is smooth and shiny, while the deeper layer has ridges that interlock with corresponding ridges on the nail bed. The nail plate is protected and surrounded by the perionychium, which seals the sides of the nail. This edge acts as a barrier against infections, damages, or allergies.
Nail Bed:
The nail bed is the adherent connective tissue located beneath the nail plate. As mentioned earlier, the deep layer of the nail plate is attached to the nail bed through complementary ridges in both areas. The hyponychium marks the transition between the nail bed and the fingertip, where the free edge of the nail begins.
How is a nail fungus infection acquired?
As mentioned before, having nail fungus is an infection caused by microorganisms. Fungi thrive in warm and moist environments and reproduce through airborne spores. When these spores find a receptive surface like the toenail, along with a suitable environment, they start to grow and multiply.
The fungi that attack the toenails feed on the nail tissues. They burrow into the skin beneath the nails, specifically the nail bed. Over time, this causes the nail to thicken until it lifts from the nail bed due to the accumulation of fungi. If the nail becomes detached, it cannot reattach itself. New nail growth will need to occur from the root, gradually occupying its place in the nail bed.
Types of fungi that affect toenails
Dermatophytes: These molds are the most common cause of nail fungus, affecting around 90% of cases. Dermatophytes feed on the keratin of the nails and typically enter through small erosions. Initially, the infection may go unnoticed, but over time, the affected nail becomes discolored, brittle, and may develop whitish deposits beneath the nail plate. Severe cases can lead to detachment of the nail.
Non-dermatophyte molds: These filamentous fungi, found in nature as soil saprophytes and plant pathogens, account for about 5% to 10% of nail fungus cases. They have limited capacity to break down keratin and infection by non-dermatophyte molds is considered less common than dermatophyte infections. Diagnostic criteria for this type of fungus are not universally agreed upon.
Yeasts: Yeast infections affect approximately 5% to 10% of individuals with nail fungus. Candida albicans is one of the most common yeasts causing onychomycosis. Yeast infections often result in inflammation, pain, and swelling around the nail. The affected nail may show ridges, yellow discoloration, or detachment from the nail bed. Women are more susceptible to yeast-related nail infections.
Overall, the acquisition of nail fungus is linked to environmental factors and the presence of specific types of fungi that invade and thrive in the nails.

Implications of Toenail Fungus
Toenail fungus has various implications that go beyond the medical aspect, addressing aesthetic, psychological, and medical concerns.
Aesthetic Implications: Toenail fungus can cause nails to become unattractive, leading to concerns about exposing them. This may result in individuals trying to hide their infected nails, hindering the healing process.
Psychological Implications: Toenail fungus can impact self-esteem due to societal misconceptions about hygiene and the infection. It may also lead to psychological distress, such as depression and difficulties in interpersonal relationships.
Medical Implications: Toenail fungus can cause pain, limit mobility, and affect the choice of footwear. It may also have implications for individuals with diabetes, potentially leading to complications like cellulitis.
Addressing toenail fungus promptly and effectively is essential to mitigate these implications and promote overall well-being.
Is it important to treat toenail fungus?
Treating toenail fungus promptly is crucial due to several reasons:
Prevalence: Toenail fungus is a common condition and the leading cause of nail diseases in developed countries. There has been a global increase in toenail fungus cases in recent years.
Diagnosis and Treatment Challenges: Toenail fungus is one of the most difficult superficial fungal infections to diagnose and treat effectively. It often requires a comprehensive approach to achieve successful outcomes.
Treatment Success Rates: It is estimated that up to 20% of patients undergoing toenail fungus treatment do not achieve complete cure. Therefore, early intervention and proper management are essential to maximize treatment effectiveness.
Emotional and Social Impact: Toenail fungus can negatively impact a person’s emotional well-being and social life. Individuals may experience self-consciousness and stigma due to misconceptions about hygiene. This can lead to social rejection and a decline in self-esteem.
Occupational Limitations: Toenail fungus can affect certain occupations that involve handling food, working in sports clubs, customer service, and more. It can cause discomfort, limit mobility, and hinder professional performance.

Causes and Risk Factors of Toenail Fungus
Several factors contribute to the proliferation of toenail fungus:
Aging: As people age, nails become more fragile and prone to dryness, creating cracks that facilitate fungal growth. Advanced age is a significant risk factor for toenail fungus.
Genetic Predisposition: Genetic factors play a role in susceptibility to toenail fungus caused by dermatophytes. Some population studies have identified a dominant autosomal transmission mode, influencing the immune response to this infection.
Inappropriate Footwear: Wearing closed-toe shoes that do not allow proper ventilation creates a warm and moist environment ideal for fungal growth. It is important to alternate between closed and open-toe footwear and choose breathable materials.
Previous Foot Fungus: Individuals who have had foot fungus in the past or currently have an active infection are more likely to develop toenail fungus. Treating and addressing foot fungus promptly can help prevent its spread to the nails.
Walking Barefoot in Public Areas: Walking barefoot in public areas like communal showers, public bathrooms, pools, gyms, and locker rooms increases the risk of fungal exposure. Using flip-flops or swim shoes is important to avoid infection.
Sharing Personal Items: Sharing personal items such as towels, socks, or shoes can facilitate fungal transmission. Direct contact with infected items increases the likelihood of acquiring toenail fungus.
Skin Conditions and Weakened Nails: Individuals with conditions like psoriasis are prone to toenail fungus due to the weakened protective barrier, making them susceptible to dermatophyte infections. Cellulitis, a bacterial skin infection, can also contribute to the development of toenail fungus.
Diabetes, Circulation Problems, and Weakened Immune System: Diabetes, poor circulation, and weakened immune systems increase the risk of toenail fungus. Individuals with HIV or other immune-weakening conditions are also more susceptible to toenail fungus.
Persistent Moisture: Poor drying of the feet and interdigital spaces, as well as wearing non-breathable socks and shoes that retain moisture, create a favorable environment for fungal growth. Those working in humid environments should take extra precautions to prevent toenail fungus due to excessive moisture.

Classification of toenail fungal infections
Clinical research has classified toenail fungal infections based on their appearance, the entry point of the fungus into the nail, and the type of infecting agent. These classifications help determine the appropriate treatment for toenail fungus. The different types of onychomycosis include:
Distal and Lateral Subungual Onychomycosis: This is the most common type of toenail fungal infection, usually caused by dermatophytes. It initially affects the hyponychium and the lateral edges of the nail. The infection then spreads proximally and is characterized by subungual hyperkeratosis. If the infection reaches the nail matrix, the nail can detach. It may be preceded by tinea pedis (athlete’s foot).
Superficial White Onychomycosis: Another type of toenail fungal infection, although less common than distal and lateral subungual onychomycosis, is also caused by dermatophytes, particularly Trichophyton mentagrophytes. It affects the surface of the nail and does not usually reach the nail bed, thus not causing complete destruction of the nail.
Proximal Subungual Onychomycosis: This type of toenail fungal infection often occurs in patients with diabetes or peripheral vascular disease. It does not present with paronychia (infection of the nail fold). Prompt treatment is necessary for individuals with these underlying conditions.
Candidal Onychomycosis: Candidal yeast infections of the nails can be classified into four main types:
Chronic paronychia with secondary nail dystrophy: It often occurs in people working in humid environments. Continuous moisture affects the nail cuticle, compromising its barrier function and leading to fungal infection.
Distal nail infection: This type of toenail fungal infection is rare and affects individuals with vascular insufficiency or Raynaud’s phenomenon. It causes minimal subungual hyperkeratosis.
Chronic mucocutaneous candidiasis: It always involves mucosal surfaces along with nail involvement. This type of toenail fungal infection occurs in patients with impaired cellular immunity.
Secondary candidal infection: This type of toenail fungal infection is associated with psoriasis.
- Onychomycosis with Total Dystrophy: This occurs when the infection is advanced and results in complete destruction of the nail plate. Any of the previously mentioned infectious types, particularly distal and lateral subungual onychomycosis, can progress to this stage.
Identifying the specific type of toenail fungal infection is crucial for tailoring the treatment approach and achieving successful outcomes. Proper diagnosis and classification help guide the selection of antifungal medications and management strategies for toenail fungus.

Who Is a Candidate for Toenail Fungus Treatment?
Candidates for toenail fungus treatment are individuals who have tried self-care measures without success and have noticed certain characteristics in their nails, such as:
- Discoloration
- Thickening
- Deformity
- Bleeding around the nail
- Swelling or pain in the surrounding skin
- Difficulty walking or wearing certain types of footwear
Suitable candidates for toenail fungus treatment can be of any age and gender. It is important to address this condition to prevent complications, as fungal infections can cause permanent damage to the nails. Moreover, they can pose a risk for more severe infections in individuals with a weakened immune system, diabetes, circulatory problems, or other underlying conditions.
Signs You Need Treatment for Toenail Fungus
Are you noticing unusual changes in your toenails? Perhaps you’re dealing with a toenail fungus infection. The most common signs that you need treatment for toenail fungus include:
Discoloration of the toenails: This could be one of the first signs. Your toenails might lose their natural color, becoming dull or taking on a different hue.
Streaks of a different color on the toenail: If you notice streaks on your toenails that contrast with their normal color, it could be an indication of toenail fungus.
Appearance of brown or yellow spots at the edges: These might be more noticeable at the edges of the nail, especially in the early stages of an infection.
Opacity in the nail: A healthy toenail should be semi-transparent. If it becomes opaque or cloudy, it’s a sign of possible toenail fungus.
Thickened and deformed toenail: Toenail fungus can cause your toenails to become unnaturally thick and misshapen, which can be both uncomfortable and noticeable.
Increased nail fragility or easy breakage: If your toenails have become brittle and prone to breaking or chipping, this could be a symptom of fungal infection.
Pain in the tips of the toes: Any discomfort or pain in the toes might be a sign of an underlying issue like toenail fungus.
Callus between the nail plate and the nail bed: A thickened skin area between your nail and the underlying tissue could indicate a fungal infection.
Crumbling of the toenail: Advanced stages of toenail fungus can cause the nail to disintegrate or crumble, often starting at the edges.
Unpleasant odor: In advanced stages of toenail fungus, you may notice an unpleasant smell coming from your feet, specifically from your toenails.
Separation between the nail and the nail bed: If you notice your toenail separating or lifting from the nail bed, it could be due to toenail fungus.
Distorted or deformed nail growth: Toenail fungus can disrupt normal nail growth, leading to distorted or deformed toenails.
If you’re experiencing these symptoms, it might be time to consider treatment for toenail fungus. Timely diagnosis and treatment can help prevent further complications, ensure healthier toenails, and increase your overall comfort and well-being.

Types of Treatments for Toenail Fungus
Toenail fungus can be stubborn to eliminate, leading many patients to try different treatments to find the most effective solution. Below we discuss some of the most commonly used and successful treatments for toenail fungus.
Medicated Nail Polishes
Over-the-counter products serve as treatments for toenail fungus, and one of them is medicated nail polish. Just like commercial color nail polishes, this is applied with a brush. But it contains an antifungal medication called ciclopirox. Once applied, the nail and its surrounding area become saturated with the antifungal medication. Patients should paint the fungus-infected nails once a day, along with the skin around these nails. After seven days of applying the polish, all overlaid layers should be removed with alcohol, and then the application starts anew. It can take up to a year for the medicated nail polish treatment to take effect, depending on the resilience of the fungus.
Prescription Topical Treatments (creams and ointments)
Antifungal creams, available both over-the-counter and by prescription, are another treatment for toenail fungus. These creams are applied to the affected nails after bathing, when the nail has been softened by soaking. This helps the medication penetrate better to reach the fungus. Topical treatment may be combined with oral medications for better results. To make these creams more effective, it’s beneficial to thin the nails – this allows the medication to penetrate the nail’s tough surface and reach the fungus beneath. You can thin your nails by applying an over-the-counter lotion that contains urea. Alternatively, a physician can thin the nail using a technique called debridement, using tools such as files.
Oral Medications
Oral antifungal drugs are often the first line of treatment for toenail fungus. This treatment is convenient for the patient, but not always the most effective. Oral medications work faster than topical ones on the infection, although they’re often combined for the best results. According to the Food and Drug Administration (FDA) statistics, oral medications eliminated the fungus in 55% to 70% of patients within ten months. However, 15% to 20% of those cured reacquired the fungus within a few months. Active ingredients used in oral antifungal drugs include terbinafine and itraconazole. These substances help eliminate the fungal infection and promote the growth of new, infection-free nails, which gradually replace the infected part. Treatment duration is usually between 6 to 12 weeks. However, the final result will only be seen once the new nail has completely grown in and replaced the damaged nail. Oral treatment for toenail fungus has a lower success rate in people over 65 years. To completely eliminate the infection, several cycles of medication intake may be required over a period of 4 to 6 months. This treatment can cause side effects such as:
- Skin rash.
- Liver damage.
- Interactions with other drugs.
- Interactions with alcohol, which should be avoided.
- Problems when exposed to sunlight.
Laser Treatment
Laser treatment for toenail fungus is undoubtedly one of the most effective treatments currently available. Laser devices used are approved by the FDA. The procedure is quick and painless, proving highly effective in eliminating toenail and fingernail fungus. The treatment works by targeting the infected area under the nail with a gentle laser that does not damage the nail structure or surrounding skin. Typically, around 4 to 5 sessions, each lasting approximately 30 minutes, are necessary for complete treatment, though this depends on the severity of the infection. Advantages of laser treatment include:
- No discomfort or pain.
- Speed and effectiveness.
- No need for oral medications that may cause side effects.
- No recovery period.
- High success rate.
- Minimal sessions required for mild infections.
- Doesn’t damage the nail or surrounding skin.
- Reaches the fungus easily, even if it’s within the nail.
- Hope for patients who haven’t been able to eliminate nail fungus with other treatments.
- Less costly than oral treatments.
Nail Removal Surgery
Another treatment option for toenail fungus is surgery. The infected nails are temporarily removed to apply antifungal medication directly to the skin, helping access the infected area beneath the nail. This procedure is conducted when the toenail fungus does not respond to other medications. In severe or painful cases, the doctor may suggest permanently removing the nail. Nail removal surgery is straightforward and performed under local anesthesia. It can be conducted in a medical office or clinic. After applying local anesthesia, the connective tissue of the nail bed is softened, and the nail is detached from the skin using a special device. The treated finger is then covered with gauze and bandages. Patients can return home the same day.

Benefits of Treatment for Toenail Fungus
- Improved Aesthetic Appeal: The treatment helps restore the healthy appearance of your toenails, adding to your overall aesthetic appeal.
- Avoids Social Stigma: The treatment helps avoid the social stigma associated with toenail fungus often linked to a lack of hygiene.
- Eliminates Pain and Limitations: It removes the pain and limitations associated with wearing certain types of footwear caused by toenail fungus.
- Removes Fear of Spreading the Infection: The treatment alleviates the fear of spreading the fungal infection to your loved ones.
- Prevents Unpleasant Odors: The treatment helps get rid of the unpleasant odors caused by the waste products of fungi.
- Enhances Social Interactions: Healthy nails improve your ability to interact with others without feeling self-conscious about your feet.
- Boosts Confidence in Interactions: You’ll notice a boost in your confidence during interactions, knowing you no longer have a fungal infection.
- Restores Nail Health: The treatment restores the health of your nail and nail bed, ensuring the future growth of your nails remains healthy.
- Prevents Deformity and Thickening: It also aids in avoiding the deformity and thickening of the nails that can occur due to untreated fungal infections.
- Allows All Kinds of Footwear: Once your toenail fungus is treated, you can comfortably wear all kinds of shoes without experiencing pain.
- Prevents Walking Discomfort: It prevents discomfort when walking, allowing you to freely engage in daily activities.
- Avoids Progression to More Serious Conditions: Treating toenail fungus helps prevent it from evolving into more serious conditions, such as peripheral circulatory disorders, diabetic foot, thrombophlebitis, and cellulitis.

10 Tips to Prevent Toenail Fungus
Due to the lengthy nature of toenail fungus treatments, prevention is key. Here are ways to deter the growth of these pesky microorganisms:
- Avoid Moisture: Keep feet dry, especially between toes after bathing.
- Wear Appropriate Footwear: Regularly switch shoes, especially closed types, to avoid creating a humid environment that encourages fungal growth.
- Protect Nails from Chemicals: Direct contact with harsh cleaning chemicals can lead to toenail damage and fungus growth.
- Change Socks Daily: Worn socks may harbor fungi, so fresh pairs are recommended every day.
- Be Cautious During Pedicures: Avoid sharing tools and be gentle while filing and cutting cuticles to prevent infection.
- Maintain Nail Hygiene: Keep nails clean and short to deter fungal growth.
- Avoid Walking Barefoot in Public: Public places like swimming pools and gym showers are hotspots for fungus, so always wear footwear.
- Treat Athlete’s Foot and Other Skin Fungi: Address skin fungi immediately to prevent them from spreading to your nails.
- Discard or Disinfect Old Shoes: Old shoes may harbor fungi, so regularly replace or disinfect them.
- Limit Use of False Nails and Nail Polish: Constant use can damage nails and create a suitable environment for fungal growth.

Risks of Treatments for Toenail Fungus
While the benefits of toenail fungus treatment undeniably outweigh the risks, it’s important to acknowledge that certain treatments, such as oral medication and surgeries, do carry some risks. However, these risks are typically minimal, and most other forms of treatment generally do not present any risks.
Risks of Oral Treatment for Toenail Fungus
The most common risks associated with oral antifungal medication for toenail fungus include the following potential side effects:
Headaches: Some people may experience headaches when taking oral antifungal medication.
Skin Irritation: This can manifest as burning sensations or itching on the skin.
Loss of Taste: Some individuals may experience a temporary loss of taste.
Nausea and Diarrhea: Some oral medications can cause feelings of sickness and diarrhea.
Liver Damage: In rare cases, oral antifungal medications can cause liver damage.
Interaction with Alcohol and Other Medications: Certain antifungal medications can interact with alcohol and other medications, making them less effective or causing other side effects.
Pregnancy Concerns: Oral antifungal medications are typically not recommended during pregnancy.
Risks of Surgery for Toenail Fungus
Surgical procedures to remove the infected toenail also carry some risks, including:
Pain: Pain can occur in the toe and surrounding area after the surgery.
Infection: There’s a risk of infection after surgery, which can be reduced by maintaining good hygiene of the area.
Abnormal Nail Growth: When the new nail grows in, there is a risk of abnormal growth.
In conclusion, while there are some risks associated with the treatments for toenail fungus, these are generally outweighed by the benefits. However, it’s always important to discuss these potential risks with your healthcare provider before beginning a new treatment regimen.
Frequently Asked Questions about Toenail Fungus Treatment at Luxe Foot Surgery
To make the most of your consultation or toenail fungus treatment, patients should consider the following:
- Remove all nail polish or artificial nails, allowing the specialist to fully examine the extent of the fungal infection and take nail samples.
- Wear comfortable clothing, as you may need to elevate your foot or lie on an examination table.
- Wear clean cotton socks and comfortable shoes.
- Maintain good foot hygiene.
Many factors can distort toenails, making it crucial for dermatologists to perform tests to diagnose if patients indeed have a fungal infection. Aging alone can thicken and yellow nails, while conditions like psoriasis can cause nail and surrounding skin scaling. Trauma can change the nail’s color and cause an under-nail hematoma, requiring different treatments.
Chemical contact, like certain nail polishes, can also discolor nails. During your consultation, the specialist will ascertain whether your nail problem has been caused by fungus or other factors.
Only through a laboratory test can a doctor determine that your nail is being attacked by a fungus and not another microorganism or factor. The usual test to identify a fungal infection involves taking a nail scraping to send to the lab. This examination will confirm if the nail distortion stems from fungus or another cause. It also allows the specialist to identify the specific fungal species attacking the nail, ensuring the right toenail fungus treatment. Misdiagnosing toenail fungus can cost time and money if ineffective products are purchased, making lab testing by a dermatologist crucial.
Most toenail fungus treatments don’t require downtime; patients can carry on with their regular activities. However, some post-treatment recommendations can help prevent reinfection and enhance treatment effectiveness:
- Wear comfortable footwear that doesn’t trap moisture or squeeze the nails.
- Avoid walking barefoot in public spaces like pools, bathrooms, gyms, etc.
- Don’t use nail polish or acrylic nails during the treatment.
- Wear breathable cotton socks.
- Change your socks daily, and wash them in boiling water.
- Wash your hands after touching the affected area to prevent spreading the fungus.
- Disinfect your shoes daily with powders or specialized spray products to prevent reinfection.
- Thoroughly dry your feet after bathing.
- Use a different towel for your feet to avoid contaminating the rest of your body.
Surgical removal of the infected toenail is the only treatment requiring recovery. After leaving the doctor’s office or clinic, patients should follow these instructions:
- The toe from which the nail was removed will be bandaged and should remain so for the first 24-48 hours.
- After this period, remove the bandages and start cleaning the wound area with clean water and neutral soap at least twice daily.
- Avoid hydrogen peroxide and alcohol as they can delay wound healing.
- After cleaning, cover the wound with a thin layer of petroleum jelly and a non-adhesive dressing.
- Repeat this procedure each time you clean the wound until the toe heals.
- The wound should heal within a few weeks. However, it can take 12-18 months for the removed toenail to regrow fully.
- During recovery, wear comfortable footwear, avoid injuring the toe, and continue with regular activities except high-impact exercises or activities involving moisture, like swimming.
The effectiveness timeline of toenail fungus treatment depends on factors such as the severity of the infection, the type of fungus involved, and its resistance. In some instances, the fungus may clear within a few weeks. However, for others, the treatment may require months of application before the fungus is eradicated. This situation can be daunting, but with patience and consistency, the fungus eventually disappears. Laser procedures are currently the most effective and fastest-acting treatments.
Finding the ideal treatment for toenail fungus can be challenging. Some patients experience lengthy recovery periods, while others quickly eliminate the fungus. The difficulty often lies in individuals self-diagnosing and resorting to over-the-counter treatments without consulting a dermatologist. Therefore, we highly recommend seeking professional assistance to receive the most accurate diagnosis. Despite this, achieving results may still take months, and reinfection can frequently occur even after successful initial treatment.
Toenail fungus infections can be recurrent, meaning they may reappear after successful treatment. As of now, no treatment can guarantee permanent eradication of toenail fungus. However, with proper care, individuals can prevent the fungus from reoccurring.
The effectiveness and duration of toenail fungus treatment vary, depending largely on the severity of the infection, the type of fungus, and its resistance level. While some instances may clear up in a few weeks, others might require several months of treatment before the fungus completely vanishes. It’s important not to lose hope, as patience and consistency are crucial to overcoming this condition. Currently, laser treatment proves to be the most efficient and fastest method.
Finding the ideal treatment for toenail fungus can be challenging, with recovery times varying from person to person. Many individuals self-treat with over-the-counter products without consulting a dermatologist, often leading to suboptimal results. We strongly recommend seeking professional advice to ensure accurate diagnosis and appropriate treatment. Be patient, as it might take months to see significant improvement, and be aware that infections can frequently reappear even after successful treatment.
Unfortunately, toenail fungus infections are recurrent in nature, meaning that they can reappear even after successful treatment. Currently, no treatment can guarantee a permanent cure from toenail fungus. However, by following proper foot care guidelines, one can significantly reduce the chances of reoccurrence.
The onset of initial symptoms is a clear sign you should consult a specialist for a toenail fungus diagnosis and treatment. Over-the-counter medications, like antifungal nail lacquers and ointments, can be used in the interim. These help to slow the fungus’s spread while waiting for a specialist appointment. But remember, early medical intervention leads to more effective outcomes, hence the importance of a prompt doctor’s visit.
Environmental and personal factors significantly influence the likelihood of developing toenail fungus. Fungi thrive in warm, moist conditions. Public places with shared facilities like swimming pools, bathrooms, locker rooms, and sports centers can significantly increase the chances of fungus spreading. Consequently, individuals who frequently visit and share such facilities are at a higher risk.
Advanced age, weakened immune systems, and certain health conditions such as diabetes and circulatory or immune system diseases increase susceptibility to toenail fungus. Women who often wear nail polish or acrylic nails are also prone to this infection because semi-permanent and permanent adhesives can weaken nails, making them more susceptible to fungal infection.
Oral medications can be highly effective for treating toenail fungus. However, they should be used under a specialist’s supervision due to potential side effects, particularly with long-term use.
Onychomycosis, or toenail fungus, is a common condition. Representing 50% of all nail diseases globally, its prevalence is increasing, particularly in developed countries. In the United States, between 2% and 3% of the population suffer from this condition. This statistic may be an underestimate as many individuals do not seek medical help.
It’s more common among older individuals and men, but can affect people of all ages and genders. Those with diabetes, circulatory issues, or immune system problems are at increased risk. It’s estimated that 1 in every 12 people worldwide suffers from some form of onychomycosis.
Generally, treatments for toenail fungus are pain-free. The exception could be surgical removal of the affected nail, performed under local anesthesia. Any post-procedure discomfort should subside within a few days.
Yes, toenail fungus is contagious. Individuals with the condition should take precautions to prevent spreading the fungus to family members at home, colleagues at work, and others in public places.
Yes, patients with toenail fungus must apply appropriate treatments to prevent the fungus from spreading. Proper hand hygiene is critical, particularly after handling the infected area, to prevent spores from lodging on another nail or skin area.
Untreated toenail fungus can exacerbate the infection, causing it to spread to other parts of the nail, the nail bed, and the surrounding skin. Over time, the nail will lose its natural shape and thicken due to accumulated fungal debris. Moreover, spores can infect nearby toenails, fingernails, and skin. An untreated fungal nail also poses an infection risk to others at home, work, or public places.
Although many people use nail polish to cover up toenail fungus for aesthetic reasons, this practice is not advisable. Nail polish traps moisture within the nail, promoting fungal proliferation. Also, the chemicals in nail polish can weaken the nail, making it more susceptible to fungal attacks. The only recommended nail polish is antifungal nail polish, a recognized toenail fungus treatment.
Toenails grow more slowly, typically taking between 12 and 18 months to regrow after fungus treatment. Fingernails grow faster, usually reappearing within approximately six months.
Antifungal nail lacquers can be effective in treating toenail fungus. However, their success depends on consistent application and the specific fungal strain. It’s important to seek specialist diagnosis and guidance before starting this treatment. Antifungal lacquers can alleviate bad odor, reduce discoloration, strengthen nails, and restore their natural appearance. They also help prevent the infection from spreading to other nails or body parts.
Urea is a highly effective topical treatment for toenail fungus. Its use on damaged, devitalized, dystrophic, and mycotic nails is well-documented in scientific literature. While its exact mechanism of action is unclear, urea is believed to have keratolytic effects, i.e., it removes scales. Urea also has hydrating effects as it breaks hydrogen bonds, softening keratin, a fungus food source. This action facilitates the deeper penetration of antifungal creams and ointments into nail layers.
Treating toenail fungus during pregnancy can be challenging as not all available treatments are suitable for use during gestation. Early medical intervention is ideal, with ointments often being more effective and safer. Medical ointments and antifungal nail polish are the safest treatments for pregnant women due to their minimal systemic absorption. However, oral antifungal medications should be avoided or limited during pregnancy as they can affect the fetus and increase malformation risks.
Maintaining good hygiene during toenail fungus treatment is crucial. It is the most effective way to prevent the infection from spreading to other nails or body parts. Furthermore, it protects those around us from contracting the infection.
Latest Articles

The Breakdown of Haglund’s Deformity Surgery Cost
Haglund’s deformity is a bony protrusion on the back of the heel. This podiatric condition is a result of calcaneus

What to Expect – Haglund’s Deformity Surgery Scar
Haglund’s deformity or syndrome is a protrusion on the back of the heel caused by an enlargement of the calcaneal

How Long Does Haglund’s Deformity Surgery Tak
Haglund’s deformity, also known as Mulholland deformity, is a bone and soft tissue abnormality on a person’s heel. It causes

Managing Pain After Haglund’s Deformity Surgery – What to Expect and Tips for Relief
Make the recovery phase after Haglund’s deformity surgery a breeze. Learn tips and tricks for managing pain after Haglund’s deformity

What to Expect After Haglund’s Deformity Surgery
When Haglund’s deformity proves to be resistant to all non-surgical remedies, such as changing footwear, anti-inflammatory drugs, and physiotherapy, surgical

Can Haglund’s Deformity Recur After Surgery? Understanding the Possibilities
When it comes to some of the most stubborn health issues, foot conditions are at the top of the list.

Haglund’s Deformity Post Surgery: A Comprehensive Guide
Each surgical procedure has a unique recovery period, no matter how minimally invasive it is. There will be certain things

What Are the Main Haglund’s Deformity Surgery Risks? An In-Depth Overview
As with any other medical procedure, Haglund’s deformity surgery comes with its own set of risks and potential complications. Before

Returning to Running After Haglund’s Deformity Surgery – A Guided Journal
When can you return to running after Haglund’s deformity surgery? Physical therapy and a smooth recovery process impact how soon
Dorsal Heel Spur Surgery – Procedure, Recovery, and What to Expect
Dorsal heel spur surgery is a procedure that alleviates irritating symptoms caused by heel spurs that develop on the back

Understanding the Costs of Laser Corn Removal
Alleviating discomfort and nagging pain caused by corns on the patient’s feet has never been easier to do. Removing painful

Minimally Invasive Hammertoe Surgery Cost – An Informative Guide
Do you need pain relief from a bent toe joint? Fortunately for many patients, there is a minimally invasive surgery