Metatarsalgia Surgery
Welcome to Luxe Foot Surgery, the premier destination for Metatarsalgia Surgery in Miami. Our state-of-the-art center boasts top-quality equipment and techniques to provide minimally invasive and effective treatments for our patients. We prioritize absolute hygiene and comfort in our clinic to ensure a humane and ethical experience for each patient. With our highly experienced doctors and specialists, we guarantee positive results and satisfaction from our patients.
Contact us by phone or through our social networks to schedule an appointment and discover the best care for your metatarsalgia needs.
AVERAGE COST
$10,000
PROCEDURE TIME
30 – 40 Min
BACK TO WORK
2 - 3 week
FULL RECOVERY
6 - 12 months
Book Your Free Consultation

Understanding Metatarsalgia: Symptoms, Causes, and Treatment
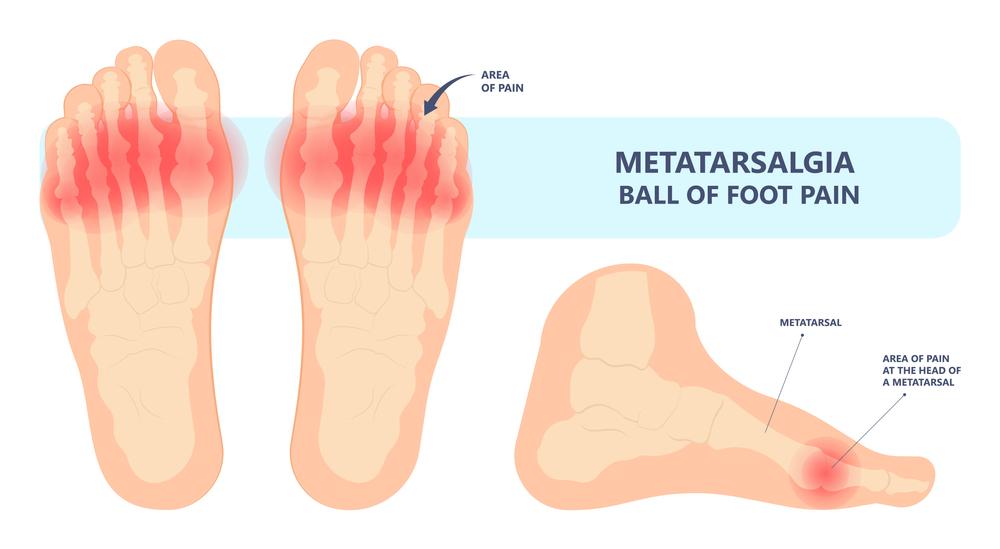
Metatarsalgia, an intricate foot condition, involves inflammation and pain in the anterior part of the foot’s sole. Initially, the condition affects the metatarsal’s bottom but can progress to the top occasionally. Although it is not classified as an ailment but a symptom, it is associated with various foot conditions.
To treat metatarsalgia, a physician must identify and diagnose the root cause of the condition. Consequently, a one-size-fits-all approach to treating the condition is inapplicable since each case presents unique characteristics. Despite the widely held belief that metatarsal bone collapse is the leading cause of metatarsalgia, the condition’s origin is the increased pressure on the metatarsal, which can have several causes, including misalignment of the metatarsals.
Metatarsalgia anatomy
Metatarsalgia’s anatomy is complex and involves the ball of the foot or the metatarsus region where the 5 metatarsophalangeal joints meet. These joints comprise the middle part of the sole of the foot, formed by the junction between the metatarsals and proximal phalanges. Weight mal-distribution results from droopy or misaligned metatarsal heads, leading to overpronation. As a result, displacement of the metatarsal bones compresses the nerve between the two bones, causing metatarsalgia or pain.
Although all the 5 metatarsals can be affected, the lower part of the second metatarsophalangeal joint is usually more commonly affected due to the area’s vulnerability to stress. However, some patients may have two or more of the 5 metatarsals affected.
Types of metatarsalgia
Specialists have described the existence of 3 different types of metatarsalgia. This classification is very useful to be able to evaluate and identify the causes of forefoot pain. In this way the doctor will be able to make a good diagnosis of the condition, and proceed to carry out the appropriate treatment. Let’s look at what the types of metatarsalgia are and what each of them consists of.
Primary Metatarsalgia
 Inflammation of the heel ligament in women due to shoes[/caption]
Inflammation of the heel ligament in women due to shoes[/caption]
Primary metatarsalgia arises from intrinsic anatomical abnormalities that affect the metatarsals. This leads to a modification in the relationship between the metatarsals and the rest of the foot’s components, causing an overload in the forefoot and resulting in metatarsalgia. The most common causes of primary metatarsalgia are:
- Having the second metatarsal bone longer than the others
- Having a cavus foot, which increases the plantar arch and produces an overload in the metatarsals
- Deformities of the middle toes
- Other anatomo-genetic deformities of the foot
- Keeping the foot in an equine-like position due to retraction of the Achilles tendon or inappropriate footwear such as high heels, which globally overloads all the metatarsal heads
Secondary Metatarsalgia
Secondary metatarsalgia appears as a consequence of alterations in other structures of the foot, causing an overload in the metatarsal as a secondary action. These alterations can lead to poor foot support, resulting in metatarsalgia. Some of the most common causes of secondary metatarsalgia are:
- Degenerative and bone pathologies such as Hallux rigidus, Hallux varus or Hallux valgus, osteonecrosis of the metatarsal heads, dislocation of the second metatarsophalangeal joint, or stress fracture of a metatarsal
- Soft tissue pathologies such as sesamoiditis, Morton’s disease, or neuroma and second space pain syndrome
- Inflammatory pathologies such as rheumatoid arthritis and bursitis
Iatrogenic Metatarsalgia
Iatrogenic metatarsalgia appears as a result of a failed surgical procedure. This causes an anatomical or biomechanical alteration of the ball of the foot or lower part of the forefoot, resulting in metatarsalgia. An example of iatrogenic metatarsalgia is when the shortening or excessive elevation of the first metatarsal occurs as a result of a failed Hallux valgus surgery, which produces an overload in the rest of the metatarsals.

How much does metatarsalgia surgery cost in Miami?
The cost of metatarsalgia surgery in Miami can range from $7,000 to $25,000. Patients with health insurance may only be required to pay a deductible, which could lead to significant savings.
The final cost of the surgery will depend on several factors:
- The type of procedure to be performed on the patient.
- The fees of the surgeon, the team of assistants and the anesthetist.
- The clinic where the operation is performed.
- The anesthesia.
- Hospital supplies.
- Additional costs, such as the purchase of crutches.
- Payment of physiotherapy for recovery.
Causes of metatarsalgia
Metatarsalgia can have multiple and diverse causes, including genetic-motor origins, bad habits, and foot diseases. However, statistics show that 92% of metatarsalgia cases are caused by biomechanical alterations. Here are some of the most common causes of this condition:
Inherited foot structure: Some people are born with abnormal foot structure and biomechanics, such as a high arch or a longer second toe. These inherited foot defects can put extra pressure on the metatarsals when walking, leading to metatarsalgia.
Condition of the metatarsal bones: When one or more metatarsal bones are too long or are not level, this can cause more pressure on them when walking, resulting in pain over the associated metatarsophalangeal joint.
Inappropriate footwear: Wearing shoes with high heels, narrow toe boxes, or inadequate cushioning can increase pressure on the metatarsals, leading to metatarsalgia.
Obesity and overweight: Excess weight can put more pressure on the metatarsals, leading to pain and discomfort.
Other foot deformities: Metatarsalgia can be a symptom or effect of other foot deformities, such as hammer toes or bunions, which can create back pressure on the metatarsal head.
Age: Advanced age can cause wear and tear on the fat pad of the foot, leading to greater pressure and pain on the ball of the foot.
Excessive use of the foot: Athletes who do a lot of jumping exercises or run frequently are more prone to metatarsalgia due to the overuse of their feet.
What is metatarsalgia surgery?
Metatarsalgia is a condition that can cause pain and discomfort in the ball of the foot. In some cases, surgery may be necessary to alleviate the symptoms. There are various types of metatarsalgia surgery, and the type performed will depend on the patient’s condition and the cause of the metatarsalgia. In this article, we will discuss the different types of surgery and their benefits.
Metatarsal Osteotomy
Metatarsal osteotomy is the most commonly used surgical procedure for treating metatarsalgia. This procedure involves cutting and reshaping the metatarsal bones to repair damaged joints. The bone is partially and carefully cut to modify its anatomical shape. There are several types of metatarsal osteotomy, including:
- Elevating osteotomy: This involves elevating the affected metatarsal bone to eliminate pressure below the joint.
- Decompression osteotomy: In this type of surgery, the metatarsal bone is shortened to relieve pressure on the metatarsal head.
- Rotational osteotomy: Also known as transpositional or Schweil surgery, this procedure involves rotating the bone to relieve symptoms and improve the appearance of the foot deformity. The bone can also be moved inward to achieve the same goal.
Metatarsalgia Surgery with Open Surgical Techniques
Open surgical techniques for metatarsalgia surgery are traditional methods that involve large incisions to access the bone for cutting according to the type of metatarsal osteotomy chosen. The bone is elevated with the installation of a pin or screw, and a process of osteosynthesis or fusion of fragmented bones is necessary to fix the implants in the bone. This type of surgery requires a longer recovery period, and patients may experience pain and swelling in the early stages. Foot rest is also needed for several weeks as premature walking may compromise osteosynthesis.
Metatarsalgia Surgery with Minimally Invasive Techniques
Minimally invasive surgery, also known as percutaneous surgery, is a delicate procedure that involves operating through minimal incisions, minimizing trauma to adjacent tissues, and reducing the risk of infections. Constant radiological visualization is necessary throughout the procedure to have precise control over surgical manoeuvres. The advantages of this type of surgery include faster recovery, less postoperative pain, better aesthetic results, and maintenance of the anatomical structures that stabilize the bony ends. However, it requires a lot of experience on the part of the surgeon, as major and even aggressive surgical operations can be performed.

How do I prepare for metatarsalgia surgery?
Here are some tips that patients should follow before metatarsalgia surgery. The objective is to be prepared so that the operation takes place in an easier and more hygienic way. Some of the indications are:
- Avoid food before surgery : Depending on the time the metatarsalgia surgery is scheduled, patients may have a light breakfast or lunch. It is recommended not to consume food about 6 hours before the operation, and not to drink liquids 2 hours before. This is to avoid digestive problems such as vomiting during the operation, as this can become a problem if the patient is anesthetized.
- Toenail hygiene : It is recommended to keep your toenails natural, well trimmed and without nail polish. This is to prevent bacteria from harboring that can later cause an infection. In addition, the nursing staff will organize an antiseptic foot bath.
- Take a companion : It is necessary to go with a companion on the day of surgery, who helps the patient to leave the clinic and can take him home. This is because the patient will most likely not be able to put their foot down to walk.
- Loose clothing : Avoid going to metatarsalgia surgery in tight clothing. The ideal is to wear a tracksuit, and in general wear loose clothing.
- No accessories : It is advisable to avoid bringing accessories on the day of metatarsalgia surgery, as they can interrupt the work of the medical team. In addition, you should avoid carrying money, coins or other objects that may fall and be forgotten.
- Do not take public transport : When returning home after metatarsalgia surgery, the patient should not take public transport, to avoid hurting his foot. Ideally, your companion should take you home in your own car. In case it is not possible, a rental car will be better.
Benefits of metatarsalgia surgery
After metatarsalgia surgery, patients need to go through a recovery period. Only then can they enjoy the benefits of the procedure. Among the main advantages of this procedure we have:
- The natural anatomy of the foot is restored.
- The tension and pressure of the body’s weight is dissipated from the metatarsal area.
- Patients are returned to normal foot functions.
- The pain and inflammation typical of metatarsalgia disappear.
- The callus on the ball of the foot is removed.
- Improves body posture and spinal alignment.
- Biomechanics and the normal distribution of plantar pressures are restored.
Metatarsalgia Surgery: Stages of Recovery
Recovery from metatarsalgia surgery is divided into several stages, in which patients must take certain care. Recovery should not be forced, since it depends on the healing processes of each organism. For example, skin healing can take about 2 weeks, while at least 6 weeks are needed for osteosynthesis or bone fusion to occur. Let’s see below some of the measures that patients must take in each stage of recovery after metatarsalgia surgery.
First day
This day it is normal to feel sore feet when the effect of anesthesia has passed. It is important that, once at home, the patient remains accompanied during the day and all night, so that someone else does what is necessary at home. In addition, the companion will be the person designated to help in the event of an allergic reaction. The patient must rest completely and keep the foot elevated for as long as possible. You cannot put your foot on the floor to go to the bathroom. As we already said, it is not advisable to bathe the first day. The use of ice packs is recommended up to 4 times a day, always avoiding wetting the bandage.
First week

In all probability, the doctor will prescribe an analgesic plan to relieve the pain from the first day and until the end of the first week. During the first 3 days of recovery, the patient should continue to rest with their feet up for as long as possible. You should avoid getting up, or only do it for essential things. These measures help prevent pain and inflammation. After the first 3 postoperative days, the patient can get up carefully, avoiding supporting the foot by using crutches and a special boot.
When bathing, you should put a waterproof bag to protect the foot and a bandage to keep it dry. The use of ice packs several times a day is recommended, always avoiding that they wet the bandage. At the end of the first week, the patient should go to the clinic for a bandage change and an inspection by the surgeon. If everything is fine, the doctor will give instructions to start making the first movements of the foot.
10 to 14 days
At this stage, the incision should have healed well, so it will be necessary to go to a second appointment with the surgeon, so that the stitches can be removed. If the sutures can dissolve, they should disappear on their own. The surgeon will give instructions to increase the level of activity with the foot. It is still not advisable to support the foot to walk, so crutches and surgical boots should continue to be used. Even though the skin is healthy, the bone continues to heal on the inside, and being overactive at this time can cause problems. The foot can already be washed during the bath.
From the fourth week
At this time, patients can return to comfortable shoes with soft cushioned soles or lace-up sneakers. However, the use of footwear will be limited, because the feet will tend to swell as the day progresses. That is why the process of wearing shoes again should be gradual, and should only increase for half an hour each day. It is normal to experience sensations such as the foot being somewhat squashed in the shoe, since the foot will have become accustomed to postoperative footwear, which is loose. It is advisable to continue using ice packs to relieve foot swelling. It is normal for the swelling to persist for several months.
From the sixth to the eighth week
In this period, most patients can expect a complete improvement of the foot. It is time to get back to work, especially those that can be seated and do not require much physical effort. People who have very active jobs should wait longer before starting work. It will still be normal to have a swollen foot towards the end of the day.
Between 6 and 12 months
At this stage of metatarsalgia surgery recovery, patients should be enjoying the benefits of it. There may be some residual, very mild swelling, or there may be no swelling at all. Complete healing is expected at this stage.
How do I know if I have metatarsalgia?
Patients with metatarsalgia problems usually present some of the following symptoms:
- They feel as if there is a rock under the toe, a sensation that is aggravated when standing or walking.
- A deep bruise may appear.
- They experience throbbing in the affected area after a very active day.
- They present a callus located under the affected metatarsophalangeal joint.
- Pain in the bottom of the ball of the foot.
- Swelling and tenderness at the top of the damaged joint.
- When the condition is very advanced, the joint capsule and ligaments in the foot can be torn, which can lead to hammer toe .
- Bursitis in the affected area of the sole of the foot.
- Burning sensation in the affected area.
- Numbness or tingling.
How does metatarsalgia affect gait?
Metatarsalgia arises from a mechanical disorder in the phases of standing while walking. This disorder is due to an imbalance in the length of the metatarsals or the angle with the floor. This anatomical anomaly causes oversupport to occur in one or more metatarsals during walking, which causes pain and calluses. To understand how metatarsalgia affects walking, one must know that the process of walking is made up of 3 phases, which are called rockers or rollers:
- Landing phase of the foot : The landing of the foot is the first rocker or roller, or the initial support, which is done only with the heel. The metatarsals do not participate in this phase. Problems such as plantar fasciitis affect this stage of the gait.
- Static phase : The static phase is the second rocker or roller. It consists of the support of the entire sole of the foot. In this phase the foot remains still and completely supported on the sole. This phase is affected by metatarsalgia to a lesser extent, although the most common problem is an increase in the angle of the metatarsal towards the ground.
- Propulsive phase : In the propulsive phase or third rocker, the heel is raised, and the entire weight of the body falls on the metatarsal heads. This is the phase most affected by metatarsalgia, especially due to the greater relative length of one or more metatarsals. This causes the weight to fall on the metatarsal during takeoff.

How is the diagnosis of metatarsalgia made?
Metatarsalgia is a painful condition that affects the ball of the foot and can be caused by various factors. To properly diagnose metatarsalgia, doctors typically follow a three-level process that includes patient history, examination, and radiographic studies.
Patient History Level
During the patient history level, the doctor will listen to the patient’s symptoms and take notes. The most significant symptom of metatarsalgia is pain in the forefoot. The doctor will inquire about the nature of the pain, such as whether it is mechanical, presents episodes of inflammation, or worsens during certain activities. Additionally, the doctor will ask about the location of the pain and any history of chronic diseases or family history of relevant conditions.
Examination Level
During the examination level, the doctor will perform physical tests to observe the actual functioning of the foot and to what extent the affectation has limited its functions. The steps of the examination include inspection, palpation, and mobility testing. Inspection involves direct observation of the affected foot to detect areas of erythema, redness, swelling, and hyperkeratosis. Palpation involves feeling for increases in temperature and identifying the areas of maximum pain when squeezing and palpating the intermetatarsal spaces. Mobility testing verifies what level of mobility the joints near the painful area have.
Radiographic Studies Level
During the radiographic studies level, the doctor will use imaging studies to confirm the diagnosis of metatarsalgia and rule out other conditions that cause the condition. Common radiographic studies include simple x-ray axial projection, ultrasounds, scintigraphies, CT scans, and MRIs. These studies can detect lesions, fractures, or other abnormalities that may be causing the pain and inflammation associated with metatarsalgia.
Overall, a combination of patient history, examination, and radiographic studies can lead to an accurate diagnosis of metatarsalgia. An accurate diagnosis is essential for developing the most effective treatment plan to alleviate symptoms and prevent the condition from worsening.
When is metatarsalgia surgery necessary?
Metatarsalgia surgery is typically considered as a last resort for patients who have not responded to non-surgical treatments after several months. In general, patients who require metatarsalgia surgery experience severe pain that limits their ability to carry out daily activities and sports. However, unnecessary surgery should be avoided, and doctors will exhaust all non-surgical options before considering surgery.
Before proceeding with metatarsalgia surgery, it is crucial to carry out detailed studies to fully understand the condition and create a surgical action plan. This helps to ensure that the surgery is necessary and that it will be effective in alleviating the patient’s symptoms. Patients and doctors must discuss the risks and benefits of surgery to make an informed decision on whether it is the best option for their specific case.

Possible risks of receiving metatarsalgia surgery
Some possible risks of receiving metatarsalgia surgery include:
Infection: Although the risk of infection is low (7.5%), it is a possible complication of any surgery. Patients should follow hygiene recommendations to reduce the risk of infection.
Recurring pain or callus: Some patients may continue to experience pain and discomfort after surgery, possibly due to a reduced range of motion in the joint. Calluses may also reappear on the ball of the foot.
Complex regional pain syndrome: This is a rare but serious complication that can result in permanent pain in the operated area.
Transfer to an adjacent metatarsal: Weight may be transferred to another metatarsal bone, which can cause metatarsalgia symptoms to appear in the adjacent joint.
Hammer toe deformity: The deformity being corrected may recur after surgery, leading to pain and limited movement.
Broken parts: Pins, screws, fixators, or other pieces installed in the osteotomy may break during the recovery period or later due to trauma. Another surgery may be necessary to remove the damaged pieces and put the bone back in place.
Lack of bone healing: Lack of or delayed bone healing is more likely in patients who smoke. Surgeons may put patients in a cast for an extended period of time to aid healing.
Nerve injury: The main nerve of the foot can be compressed during surgery, leading to temporary or permanent cramps and lack of sensation.
Incision with delayed healing: Patients may experience a thickened and tender scar with areas of numbness near the scar that can take up to 12 months to heal.
Deep venous thrombosis: The formation of blood clots in the leg is a rare but potentially life-threatening complication. Surgeons may prescribe medication to prevent this in patients with a history or risk of DVT.
What can I expect from metatarsalgia surgery?
During the recovery period, patients may experience pain and swelling in the operated foot. The surgeon may prescribe pain medications to alleviate this discomfort. Patients will also need to keep the foot elevated and avoid putting weight on it for a period of time. The length of time will depend on the type of surgery performed and the extent of the procedure.
The patient may need to use crutches or a wheelchair to move around during the first few weeks of recovery. The surgeon will provide instructions on when the patient can resume regular activities and return to work. This may take several weeks to a few months.
Physical therapy may be recommended to help restore range of motion and strength to the foot and ankle. The therapist may also teach exercises to prevent future foot problems.
It is important to follow all post-operative instructions provided by the surgeon and attend follow-up appointments to ensure proper healing and to monitor for any complications. With proper care and attention, most patients can expect a successful outcome from metatarsalgia surgery and a return to normal activities.

Exercises for recovery from metatarsalgia surgery
During the recovery period, patients must follow a simple exercise plan. These aim to keep the foot moving and with good circulation. In this way the muscles are exercised and blood clots are avoided. These exercises will become more complex as the days go by. Let’s see what they consist of:
- From the first day of recovery, it is important to move your feet up and down 15 times in a row every 30 minutes.
- From the third day (if the foot did not have some type of wire protruding from the toe attached), the patient can begin to gently move the toes. It is convenient to maintain this movement for 2 minutes and do the repetitions 5 times a day.
- When the incision is healed and the stitches have been removed, the patient can begin to move the operated toe with his hand, making gentle movements: Stretch the toe forward as much as possible, and when you feel uncomfortable return to the starting position. Then, stretch the toe back, as much as possible, and when you feel discomfort, return it to the starting position. You have to do 10 repetitions of this exercise, for each direction in which you stretch your finger, 3 times a day.
- If the surgeon gave the patient a splint, he must use it for the estimated time.
Non-surgical conservative treatments for metatarsalgia
There is a wide protocol of non-surgical or conservative treatments to improve the condition of metatarsalgia. The first thing the doctor will tell you is to follow some of the conservative treatments for 2 or 3 months. Most patients feel an improvement in symptoms after this time. The objective of this type of treatment is to reduce the pressure in the affected area. Those who do not perceive an improvement after practicing these treatments, may need metatarsalgia surgery. Let’s look at some of the most commonly used non-surgical methods for metatarsalgia.
Shoe padding

The use of accessories such as pads to cushion the shoes inside is highly recommended. They can be easily found in the market. Toe-cap metatarsal pads, which are composed of silicone gel, are also recommended.
Consumption of pain medications
When metatarsalgia pain begins, many patients turn to pain medication. The most popular of all is over-the-counter ibuprofen. It can be consumed up to 3 times a day with each meal, in doses of 200 mg. If an adequate anti-inflammatory effect is to be obtained, this dosing pattern should be maintained for 10 consecutive days. Ibuprofen is contraindicated for some health conditions, such as:
- kidney defect
- stomach ulcer
- diabetes mellitus
- The bleeding disorder
Ibuprofen is also incompatible with other medications, and can cause side effects. We recommend going to the doctor before taking ibuprofen.
Use of orthoses or orthopedic devices
Orthoses or orthopedic devices for the feet are made to measure. The doctor sends them to be done in a laboratory in a personalized way, with the aim of solving the needs of each patient. Forefoot extensions that are designed to “float” and take weight off the metatarsal bone can also be added to orthotics. The benefits of orthotics and orthotic devices are that they:
- They control the function of the foot.
- They relieve the symptoms of metatarsalgia.
- They help keep the foot in a more comfortable position.
- They prevent the worsening of the condition.
- They minimize the pressure of the body on the foot.
- They redistribute weight over the painful area.
Appropriate shoes

The most appropriate footwear to improve metatarsalgia is the one with a well-cushioned sole. Shoes designed with a rocker sole are also recommended, such as those of the following brands:
- Skechers
- Shapeups
- mbt
The shoes that should be avoided when there is metatarsalgia are those with high heels and those with hard soles, because they do not have good cushioning.
Maintain callus care
It is important to keep calluses well cared for, to prevent them from growing so much that they hurt the foot more. They can be cleaned once a week, at home or at a podiatrist. They can be trimmed or filed down with a pumice stone or callus file.
Physiotherapy treatments
There are several physiotherapy treatments to alleviate the symptoms of metatarsalgia. Some of them foster such a remarkably positive state in the foot that they manage to avoid metatarsalgia surgery. The therapies that have given the best results are ultrasound and the application of interferential electrical current. Both treatments are very beneficial in reducing inflammation and pain.
Cortisone injections
Cortisone injections help patients with metatarsalgia to reduce inflammation and speed up the recovery process. Injections are applied directly to the affected area. They are usually combined with other non-surgical methods, such as changing the type of shoes, orthotics, stretching exercises, etc. Although cortisone injections are very effective, it is not good to abuse them, since they can cause some imbalances, such as:
- Increased pain in the first 24 to 72 hours after giving the injection.
- Atrophy of the fat pad of the foot.
- Depigmentation of the upper part of the forefoot.
- Weakening of the adjacent articular ligaments.
- Possible toe dislocation.
- Infection.
Permanently immobilize the foot with a cast
Keeping the foot immobilized for a while, even without trauma, helps to improve symptoms such as pain and inflammation. Casting is the most effective way to keep your foot temporarily immobile. This complete rest of the foot, and the rest from not supporting it, relieves metatarsalgia. When the cast is removed, use of the correct footwear and other conservative methods should be maintained.
Frequently Asked Questions
The total recovery time ranges between 3, 6 and 12 months, depending on the conditions and the recovery rate of each patient. Recovery is one of the most important moments of the process. A good part of the success of metatarsalgia surgery depends on following the relevant indications for each stage of recovery.
It is estimated that around 10% of the world’s population suffers from metatarsalgia, and that 80% of the total population may experience metatarsalgia symptoms at some point in their lives. Statistics show that 88.5% of people with metatarsalgia are adult women. The factors that most influence this population group are usually the frequent use of high-heeled footwear, which creates biomechanical alterations in the foot. Keeping the foot in the so-called “equine position” (resting on the metatarsus), unbalances the distribution of the body’s overload, and exerts greater pressure on the metatarsals. Metatarsalgia is also due to a certain genetic predisposition, but this cause is much less frequent than the use of inappropriate footwear.
There are some methods that we can put into practice at home to improve the symptoms of metatarsalgia. Some of the most common methods are:
- Put ice on the painful area : Ice is convenient to relieve pain and inflammation. An ice pack should be applied where the foot is most painful. From 2 to 3 times a day you can put an ice pack between 15 and 20 minutes. You can massage the area with ice, or place your foot on it. It is more advisable to apply ice at night, when the foot is going to remain at rest. This method is not recommended for people who have circulation or sensitivity problems.
- Decrease the number of activities : Foot rest is a good way to avoid the aches and pains of metatarsalgia. Likewise, some positions should be avoided, such as squatting, standing on tiptoes, walking downhill or wearing high heels that keep the foot in an equine position.
- Avoid high-impact exercises : To prevent pain from worsening, it is recommended to stop doing high-impact exercises, that is, those that demand a lot of strength and are very intense, such as: running, playing soccer, lifting weights, etc. It is better to do low-impact exercises, such as swimming, bicycling or running in the pool.
- Immobilize the foot : The doctor can teach the patient some splinting or padding techniques, so that the foot can be immobilized at home for as long as he wants, without having to go to the clinic for it. This immobilization can be done for a full day, or for a few hours.
- Practice stretching exercises : Stretching exercises for the calf muscles can be done every day at home. At least 2 times a day, repetitions of 30 to 60 seconds can be done for each foot. The exercise consists of standing in front of the wall supporting both palms of the hands perpendicularly against the wall. Then you have to bend one leg forward, while the other remains stretched behind. In this way, swing the body forward as much as possible without separating the soles of the feet from the ground. When the patient feels the tension in the calf of the foot that has been left behind, they should hold the position for 30 to 60 seconds, before moving to the other foot to do the same.
For metatarsalgia surgery, local anesthesia is used, which may be accompanied by sedation under the control of an anesthetist. Usually the foot remains asleep for a period of 4 to 6 hours. This gives the perfect period of time to perform the metatarsalgia surgery without the danger of the effect of anesthesia wearing off, and to avoid pain for a while.

After the first 2 days, or in some cases after a week after metatarsalgia surgery, patients are recommended to start washing the wound. Performing foot baths with saline solutions in warm water every day will be very useful.
To prepare this solution, water must be boiled and allowed to cool in the container where the foot will be placed. You have to wait for the water to reach a temperature that allows you to insert your hand without hurting yourself. That’s the time to add a tablespoon or two of common salt. The foot should not be soaked for more than 5 minutes in this saline solution. If there are pieces of bandage stuck to the wound, they should be allowed to get wet and fall off on their own. When finished, the foot can be bandaged with thin gauze or left in the open air.
When the person goes to the consultation for the first time, the doctor will ask several questions, with the aim of knowing the history of the possible patient. The person should express as clearly as possible the symptoms they feel when walking or doing other activities. You must also say if you have any disease. Then the doctor will do an examination of the foot, which includes both tests to determine the real mobility of the foot, as well as palpate the affected areas to recognize them. Finally he will indicate some x-rays. Then you can issue an accurate diagnosis of the causes of metatarsalgia and possible solutions, whether non-surgical or surgical.
Patients who have a type of work that does not require much physical effort can begin their activities between the fourth and sixth week of recovery, while always keeping the foot as carefully as possible. On the other hand, patients who have a heavier job that requires more physical effort must wait until the sixth or eighth week to return to work.
After metatarsalgia surgery, patients will be able to return to so-called “low impact” exercises after the third week of recovery. Riding a bicycle or exercising in the pool are optimal exercises for this stage. High-impact exercises and sports, which include jumping, running, or doing a lot of physical effort, can begin to be practiced from the third or fourth month. But if the patient is still not completely recovered, he must wait until the sixth month to carry out these practices. Before beginning any physical practice, you must ask the opinion of the surgeon.
After the sixth or eighth week of recovery, metatarsalgia surgery patients may be ready to drive. Although the foot may still be inflamed, normal footwear can now be used (if it fits), and the person will have enough strength to perform the maneuvers on the car pedals. However, we recommend that the patient consult with their surgeon before starting to drive. There are people who need to wait a little longer before driving, and complying with that may depend on the smooth recovery. In addition, it is convenient to ask the car insurance about the basic conditions that people who have recently had foot surgery must meet to maintain coverage.

In the event of any unusual signs, patients should immediately contact their surgeon. Some of the symptoms that recovery after metatarsalgia surgery is not going well are the following:
- Swelling beyond normal.
- Purple and red foot.
- Itching and burning in the wound area.
- Release of pus or blood that wets the bandages.
- Continuous fever that does not go down.
- Signs of bad odor in the surgery area.
Statistics show a 75% success rate for metatarsalgia surgery. Of the remaining 25% of people who receive surgery, 20% feel improvements, although they maintain some limitations in the use of footwear and their daily activities. The other 5% do not improve or worsen their initial condition. From this we can conclude that metatarsalgia surgery does have a high success rate.
Foot surgeries tend to have a very bad reputation when it comes to pain. But the truth is that, with highly specialized surgical and anesthetic techniques, the pain will not be too much. During the surgical procedure, the patient will not feel anything, since the foot will remain under the effect of local anesthesia for more than 4 hours. The pain will begin to be felt when the patient is at home, and the effect of the anesthesia has passed. It is normal to feel pain and discomfort for the first few days. However, the doctor will indicate what to do to minimize the pain, in addition to prescribing an analgesic plan. After the first week of recovery, the pain will decrease significantly, until it disappears as the days progress.
After metatarsalgia surgery, it is important to follow the guidelines for the early stages of recovery. Complying with them will allow the surgery to have been worth it at the end of the convalescence period. Some of the things that the patient can and cannot do after surgery are the following:
- Do not support the weight of the body on the affected foot, until the surgeon indicates.
- Avoid walking for the indicated time. Only walk for really necessary things.
- If the patient needs to walk, they should use crutches or trauma shoes.
- When you get home after surgery, the patient should keep the foot elevated for as long as possible for several days.
- Do not take public transport, to avoid injuring the operated foot.
- Come with a companion to metatarsalgia surgery.
- Stay at home when the operation is over.
- Have someone accompany you during the first days of recovery.
- Do not drive until the doctor tells you to.
- If you can’t find someone who can stay at home, the patient must stay at someone else’s house.
- Keep the foot with the bandage that is placed after surgery, until the surgeon removes it.
- Do not wet the foot or wash it until the surgeon tells you to.
- Call a doctor right away if the bandage comes loose or if there is bleeding.
- Put your foot up as long as possible from the first day and during the first weeks.
- Avoid climbing stairs. Only do it if absolutely necessary.
- Apply ice packs (without wetting the bandage) every day every 4 hours. Put them on top of the bandage.
From the third week, when the surgeon has already removed the stitches from the wound, patients will be able to take their first steps. In the fourth or sixth week, you can begin to wear normal shoes, if appropriate. It is common for the foot to swell in the afternoon and at night. To minimize this, you should alternate between resting and walking so that you don’t overstrain the area of the operation.
- JL Besse. Metatarsalgia. Sciencedirect. 2017. Available from: https://www.sciencedirect.com/science/article/pii/S187705681630189X
- Naranjo-Ruiz C, Martínez-Nova A, Canel-Pérez MA, López-Vigil M, Ferrer-Torregrosa J, Barrios C. Influence of Foot Type on the Clinical Outcome of Minimally Invasive Surgery for Metatarsalgia. A Prospective Pilot Study. Int J Surg Res Pract. 2021; 8(2): 32-39. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8490922/
- López-Vigil M, Suárez-Garnacho S, Martín V, Naranjo-Ruiz C, Rodríguez C. Evaluation of Results after Distal Metatarsal Osteotomy by Minimally Invasive Surgery for the Treatment of Metatarsalgia: Patient and Anatomical Pieces Study. J Orthop Surg Res. 2019; 14(1): 126. Available from: https://josr-online.biomedcentral.com/articles/10.1186/s13018-019-1159-0
- Amaha K. Conservative Treatment for Primary Metatarsalgia. Orthopaedic Journal of Sports Medicine. 2018; 6(2): 2325967118756574. Available from: https://www.orthojournal.org/articles/conservative-treatment-for-primary-metatarsalgia.html
- Patil S, Hanumantharaya GH, Desai SP, Nidoni M. Radiological Biometric Study of Metatarsals and Phalanges. J Clin Diagn Res. 2017; 11(9): AC05-AC08. Available from: https://www.jcdr.net/article_fulltext.asp?issn=0973-709x&year=2017&month=September&volume=11&issue=9&page=AC05&id=10589
Latest Articles

Toe lengthening surgery before and after
Toe lengthening surgery, also known as toe augmentation or toe shortening surgery, is a procedure aimed at altering the length

Metatarsal lengthening surgery
Metatarsal lengthening surgery is a procedure performed to address conditions such as metatarsalgia or a shortened metatarsal bone. It involves

Toe Lengthening Surgery in New York and Miami
Toe lengthening surgery is a procedure designed to increase the length of one or more toes and improve their appearance

Toe Lengthening and Prosthetic Nail Surgery
Toe lengthening and prosthetic nail surgery are two types of foot surgeries that can be used to address a variety

Does Toe Lengthening Surgery Hurt
Before every medical procedure, the patients usually create a pros and cons list in their heads to weigh out if

Walking After Toe Lengthening Surgery
Most people that are unsatisfied with their toes think about toe lengthening surgery at some point. The first thing that

Toe Lengthening Without Surgery
If you are struggling with brachymetatarsia, otherwise known as a short toe, you must be wondering – is toe lengthening

Toe Lengthening Surgery Recovery Time
Brachymetatarsia, otherwise known as a short toe, is a foot condition caused by stunted growth of one of the metatarsal

Toe Lengthening Procedure
The toe lengthening procedure, also known as toe augmentation or toe extension, is a type of surgical procedure that aims

Heel Cord Lengthening Surgery for Toe Walking
Toe walking is a condition that can occur in some children. It can be idiopathic or due to an underlying

Toe Extensor Tendon Lengthening CPT
If you’ve been experiencing chronic pain and having trouble with walking and the appearance of your feet because of your

Heel Cord Lengthening and Toe Pins – What You Should Know
Heel cord lengthening and toe pins, also known as the Achilles tendon lengthening surgery, is a medical procedure where, as